Start4Life launches new Breastfeeding Friend tool on Google Assistant during World Breastfeeding Week
As World Breastfeeding Week launches (1 August), the 24/7 Breastfeeding Friend from Public Health England’s programme Start4Life has been made available on Google Home and the Google Assistant app for mobile to provide even more parents with advice and support during the first few weeks of breastfeeding.

Start4Life Google Assistant
The 24/7 Breastfeeding Friend has been developed to provide friendly advice to mums who have questions and need support with breastfeeding at any point day or night. The tool is voice activated on the Google Assistant app and Google Home, meaning mums can get NHS-approved advice and daily breastfeeding tips in the moment and when they may have their hands full. Anyone with a smartphone can download the Google Assistant app for free and say “Hey Google, talk to Breastfeeding Friend” to access the service. Those with a Google Home device set up can access the service with the same phrase.

Start4Life Google Assistant
The 24/7 Breastfeeding Friend is also available on Amazon Alexa and Facebook Messenger and joins a suite of breastfeeding tools from Start4Life, including the relaunched Start4Life website, the ‘Off to the Best Start’ breastfeeding leaflet and the Start4Life Information Service for Parents, all of which provide 24/7 access to expert NHS advice and useful information, in a friendly and accessible way.
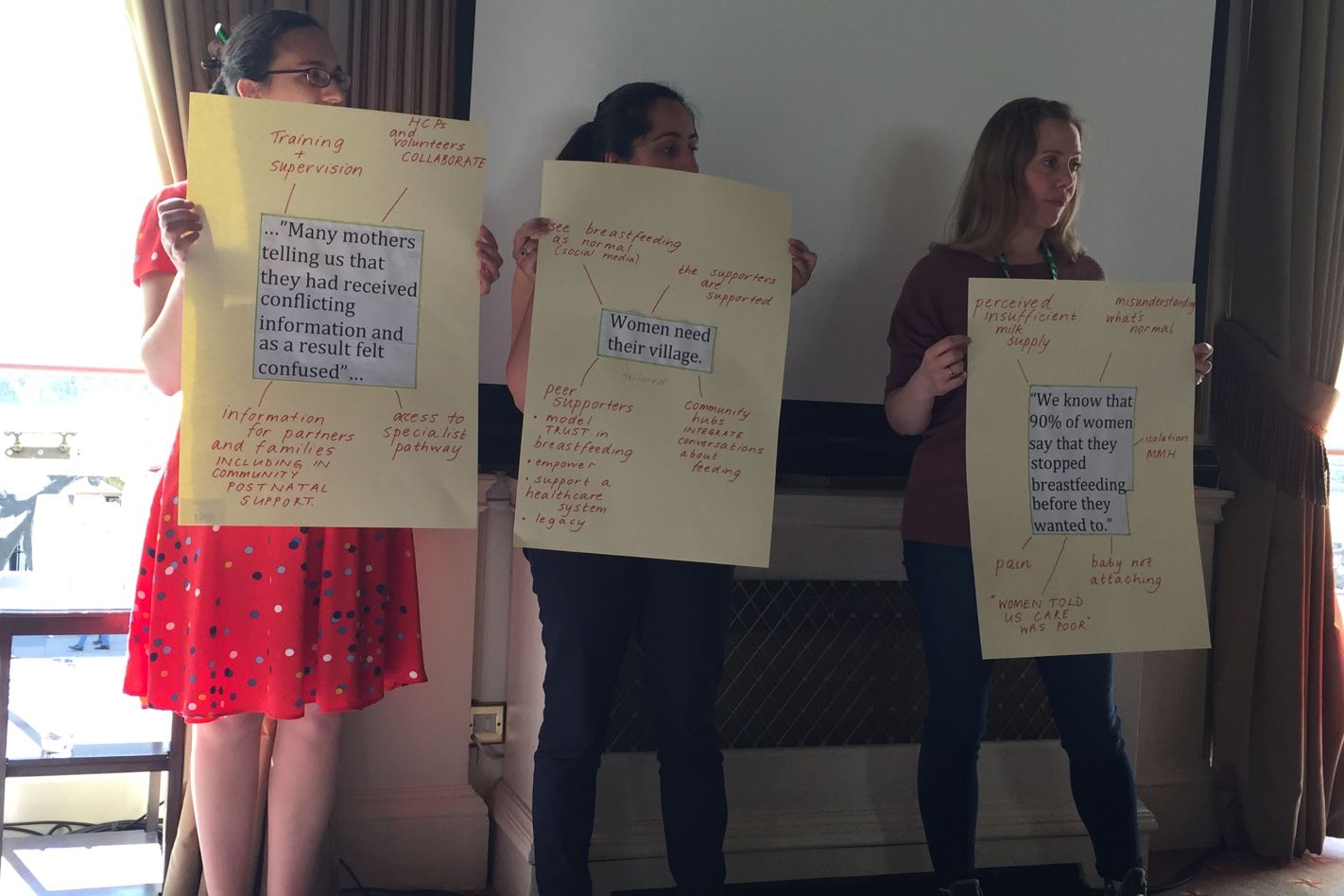
Whilst three-quarters of women start breastfeeding when their child is born, by 6-8 weeks this drops to just 44%[1] , making breastfeeding rates in England amongst the lowest in the world.
However, new research[2] among 1,000 mothers commissioned by Public Health England shows that 42% of breastfeeding mums wish they had known that breastfeeding may not come easy at first but getting support and advice can really help. When mothers reflected on breastfeeding, the poll also illustrated that 26% wished they had known that asking for help breastfeeding can make a real difference. Almost one in four (24%) wish they had known that there is lots of help and support from breastfeeding groups, other parents and online.
Public Health England recommends exclusive breastfeeding for around the first six months. Breastfeeding boosts a baby’s ability to fight illness and infection, and babies who are not breastfed are more likely to get diarrhoea and chest infections. Breastfeeding also lowers a mother’s risk of breast cancer and may reduce the risk of ovarian cancer.
[1] Public Health England annual data on breastfeeding at 6-8 weeks
[2] Kantar data collected from 1,005 mothers of children under the age of 4 on behalf of PHE, 26th January to 7th February 2018