At the start of the UK Maternal Mental Health Awareness Week (4-10 May 2020) with the theme of ‘Supporting mums during difficult times’, a blog by Melita Walker, Mental Health Lead at the Institute of Health Visiting , to highlight the essential work of health visitors in supporting mums’ and families’ mental health needs – and a call to join us in recognising and appreciating all Mental Health Practitioners as key frontline workers at 8pm this Thursday #ClapForMentalHealthHeroes @ClapforCarers @ClapForKeyworkers.

iHV clapping our Mental Health Workers
This Thursday at 8pm, like the previous Thursdays, the Institute of Health Visiting will be joining the national wave of appreciation for our courageous frontline workers. However, this week as part of Maternal Mental Health Week, we particularly want to recognise and honour the determined efforts of the iHV Perinatal and Infant Mental Health Champions and all those who have been working tirelessly alongside them throughout this pandemic, to prioritise and ensure that the mental health needs of families are effectively and proactively responded to during this pandemic.
The perinatal period, whilst often being one of great joy, is also an increased time of risk and vulnerability. Latest UK research suggests that:
- 1 in 4 women are affected by perinatal mental health disorders
- Maternal suicide is the leading cause of death when looked at over the perinatal period
- Approximately 10% fathers experience perinatal mental illness (PMI) but 25-50% of fathers will experience perinatal anxiety or depression when the mother also has a PMI
The impact on the foetus or the infant/child who has a parent experiencing mental illness is not inevitably negative, but they are at increased risk for a range of poorer outcomes and it is essential that we make sure their voice is heard and that we are proactive and act to support families at the earliest opportunity.
At the moment, parents are having to negotiate the usual associated changes that becoming a parent involves (physiological, psychological, environmental, social and emotional changes) alongside reduced family, friend and service support and other increased worries, stress and impact caused by the COVID-19 pandemic.
“How it feels to be 29 weeks pregnant amid COVID-19, a thread…Truly I have no idea how I am supposed to feel. At first, I was really calm and over the last few days everything has changed. I am scared, I am anxious”.
As the country faces its biggest challenge in recent memory, the primary focus has been to stop the spread of the coronavirus and treat infected patients. This has required a rapid increase in staff required for frontline duties and, understandably, this is a priority. Attention is now turning to the secondary impacts of the pandemic, including the mental health and wellbeing of our children and their families. They too are at immediate risk and they cannot wait for support.
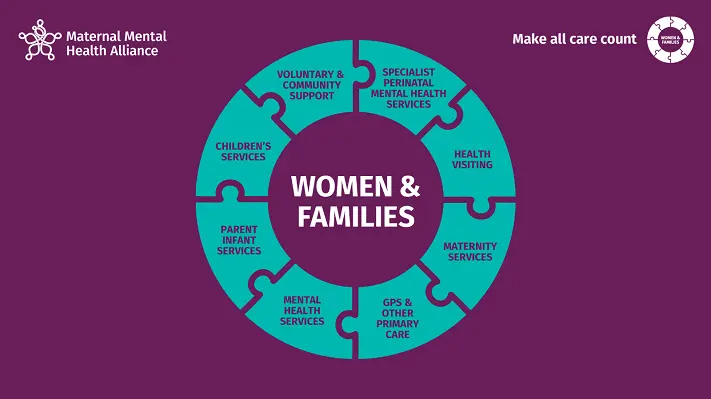
As this pandemic is global in its reach, learning from previous pandemics and other countries’ current experiences of the secondary impact of COVID-19 suggest that the pandemic is likely to have more adverse effects for vulnerable parents and children, with domestic violence and abuse, safeguarding and mental health needs of vulnerable populations likely to increase as the crisis continues. It is therefore imperative that the national response to COVID-19 incorporates both the immediate focus to treat people who are infected with the coronavirus, as well as children and families at risk from the secondary impact of the pandemic. We ignore, at our peril, the impact of not seeing perinatal and infant mental health (PIMH) practitioners as frontline workers in the fight against COVID-19.
The iHV has trained 2095 multi-agency PIMH Champions and we are hearing the voices from professionals across the range of PIMH systems and services and from parents with needs across the mental health spectrum of care. Parents are telling us that they are anxious – we know for some that the current situation is triggering new episodes of illness and for others exacerbating illness already there, and we are hearing that parents feel unsure about reaching out for support.
Eve Canavan BEM, Coordinator- UK maternal mental health awareness week, Perinatal Mental Health Partnership, commented:
“The Perinatal Mental Health Partnership have received feedback from mums and families of the uncertainty surrounding what support is available from health care professionals at this unusual time, with a clear message coming through that those who require support are unsure if they can contact their GP, midwife, health visitor or local mental health services. This means some women may not be currently accessing support they need. The stigma surrounding mental health and the perception that services are so overstretched and unsafe means that many mums are struggling but do not feel they have the right to ask for the help that they need. We are delighted to be working with the iHV and other key stakeholders during Maternal Mental Health week to get the message out that family mental health is a priority and that services to support families are very much open for business”.
We are hearing from professionals whose concerns include, worry about:
- hidden and unmet need
- risk of suicide
- the immediate safety of women and their unborn babies/infants/children
- the potential impact of untreated mental health problems/illness on the unborn baby, developing infant and older children
- the impact of the current stress that families are experiencing on the couple relationship/ couple conflict and domestic violence and abuse.
“Its really important to consider the impact of changes in working practices and redeployment of staff who play a vital role in in assessment, monitoring and onward referral for mums mental health. Some perinatal mental health conditions develop rapidly and without warning and families need urgent help”.
We are hearing that some PIMH practitioners have been redeployed while at the same time we are hearing that parents and their children need them now, and more than ever. We are also hearing of practitioners and services that continue to see the vital importance of prioritising mental health and from parents who say that they are a lifeline.
“I am pleased to say XXX health visiting service is increasing. 34 staff are being redeployed back in from various services within the trust. Health Visiting in XXX is considered critical to life service at the moment”.
“Now reassuring pregnant and postnatal mums, some of whom are fearful of attending hospital for maternity care. Please continue to keep antenatal appointments, scans and sharing worries and concerns with your midwife, it is safe to do so. If something doesn’t feel right, call you midwife”.
“Met my HV over the phone today- so knowledgeable, professional and kind!! Thankful for such a simple adjustment to practice that is reassuring for newbie mums”.
What can we do to support perinatal and infant mental health at this time?
The iHV will do all we can to support our PIMH Champions and colleagues working across the PIMH spectrum. We will continue to collaborate nationally, to support all families locally.
We have developed a comprehensive compendium of resources for professionals and families:
We are regularly updating these pages, so please keep checking back for the latest!
Let’s hear it for Family Perinatal Mental Health – this Thursday!
Maternal Mental Health , with its theme of “how to support mums through difficult times”, is a great opportunity to raise the importance of family mental health and to let families know what support is out there. It was brilliant to have the profile of perinatal mental health raised by the Duchess of Cambridge over weekend, and it has been wonderful to work alongside so many individuals, organisations, professionals, parents and alliances to highlight the need for supporting family mental health.
We look forward to sharing more of the fantastic examples of the responses and efforts from our frontline mental health practitioners to support family mental health during Maternal Mental Health week. Mental health practitioners are frontline now, and crucially, will be needed on the frontline (dealing with the psychological aftermath of COVID-19), long after any vaccine has brought the coronairus under control.
We do hope you will join us in recognising and appreciating all Mental Health Practitioners as key frontline workers at 8pm this Thursday #ClapForMentalHealthHeroes @ClapforCarers @ClapForKeyworkers
Melita Walker, Mental Health Lead at the Institute of Health Visiting