The mental health of babies and young children is important for their wellbeing now, and critical for their future health and development. These earliest years are a time of rapid development and offer the best chance to lay strong foundations for good mental health. Many people, however, do not really know what being mentally healthy means, especially for babies and young children.
The iHV is delighted to support today’s launch of UNICEF UK and The University of Cambridge Play in Education, Development & Learning (PEDAL) Centre’s new resource ‘Understanding and supporting mental health in infancy and early childhood -a toolkit to support local action in the UK’ that aims to promote a shared understanding of what is meant by mental health in the early years.
Hilda Beauchamp, Perinatal and Infant Mental Health Lead at iHV, said:
“We have been privileged to collaborate with UNICEF UK and PEDAL to produce this important toolkit, highlighting what can be done to support babies’ and young children’s mental health and wellbeing. Health visitors have a vital role to play in ensuring that all babies grow up being mentally healthy: able to understand and manage their emotions, experience nurturing relationships and be able to explore, play and learn.
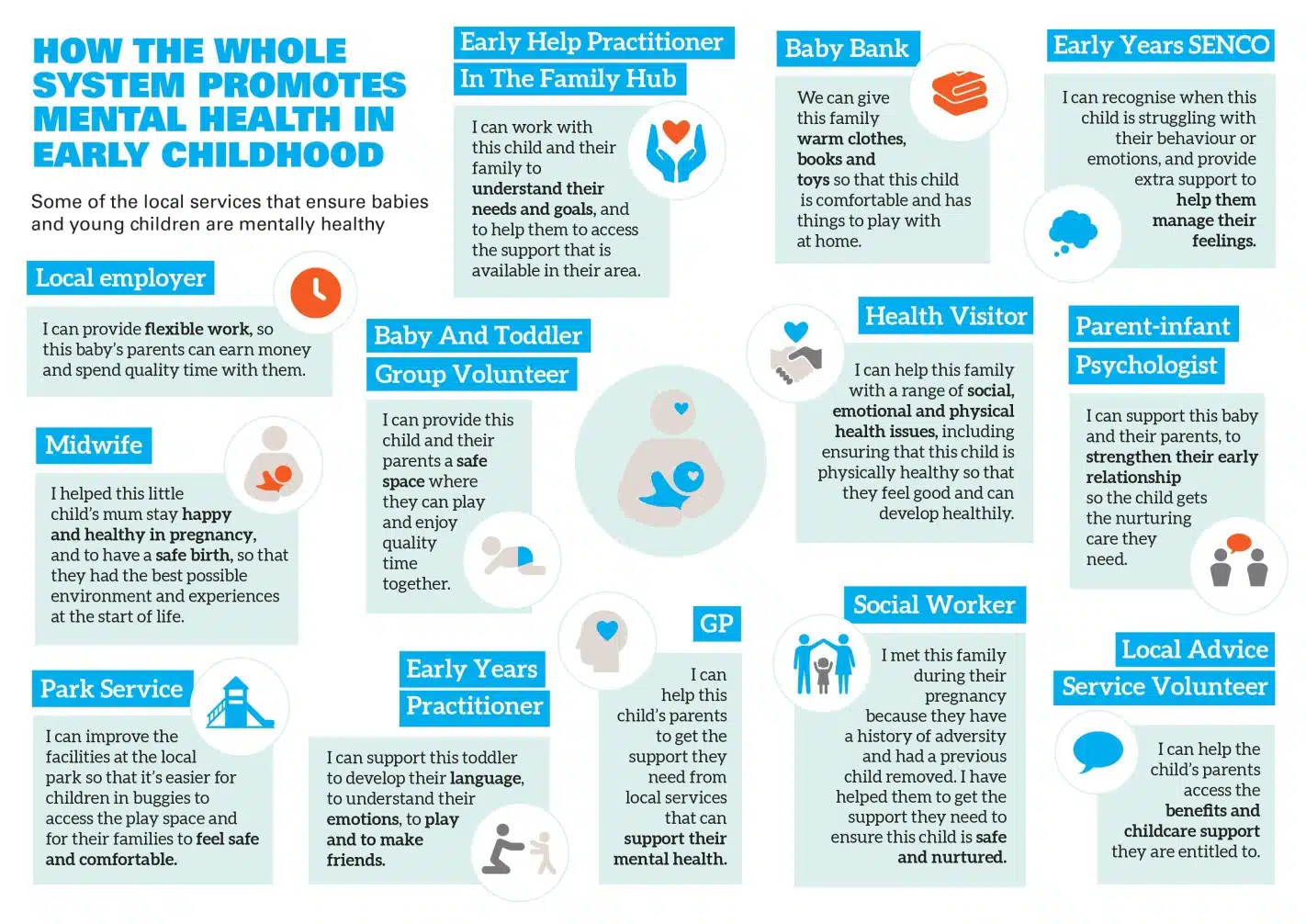
“This toolkit will help to ensure a more effective whole system approach for health visitors to work alongside their multi-agency colleagues in developing a shared understanding of babies’ and young children’s mental health and see the contributions they can make. Supporting multi-sector working, along with addressing inequalities that affect families, can help to give babies and young children the best start in life.”
The toolkit aims to:
- Help partners from different services and professions to develop a deeper, shared understanding of mental health in infancy and early childhood, and the factors that influence it
- Support service leaders, commissioners and other decision makers and policy teams to develop whole-system responses to ensure babies and young children are mentally healthy now and are supported to develop the skills they need to continue to be mentally healthy throughout their lives
- Provide resources, signposting, and conversation guides to support constructive local discussions, decisions and action about the needs of babies and young children in their area, and what more might be done to respond to these needs (including through strategy development across mental health, maternity, early years or Family Hubs and Start for Life).