Child health is suffering at the hands of a disjointed approach from central Government is the warning from the Royal College of Paediatrics and Child Health (RCPCH) as it publishes its “State of Child Health: One year on” scorecard today.
The scorecards for England, Scotland and Wales describe progress against the series of recommendations made a year ago in the RCPCH’s landmark State of Child Health report.
The England scorecard reveals progress in some areas including the launch of a Digital Child Health Strategy, the publication of a new Tobacco Control Plan, the initiation of some specialist service reviews in paediatrics and the implementation of the sugar tax. However, there has been no improvement in several fundamental areas, including:
- No plans for an overarching child health strategy
- No junk food advertising ban
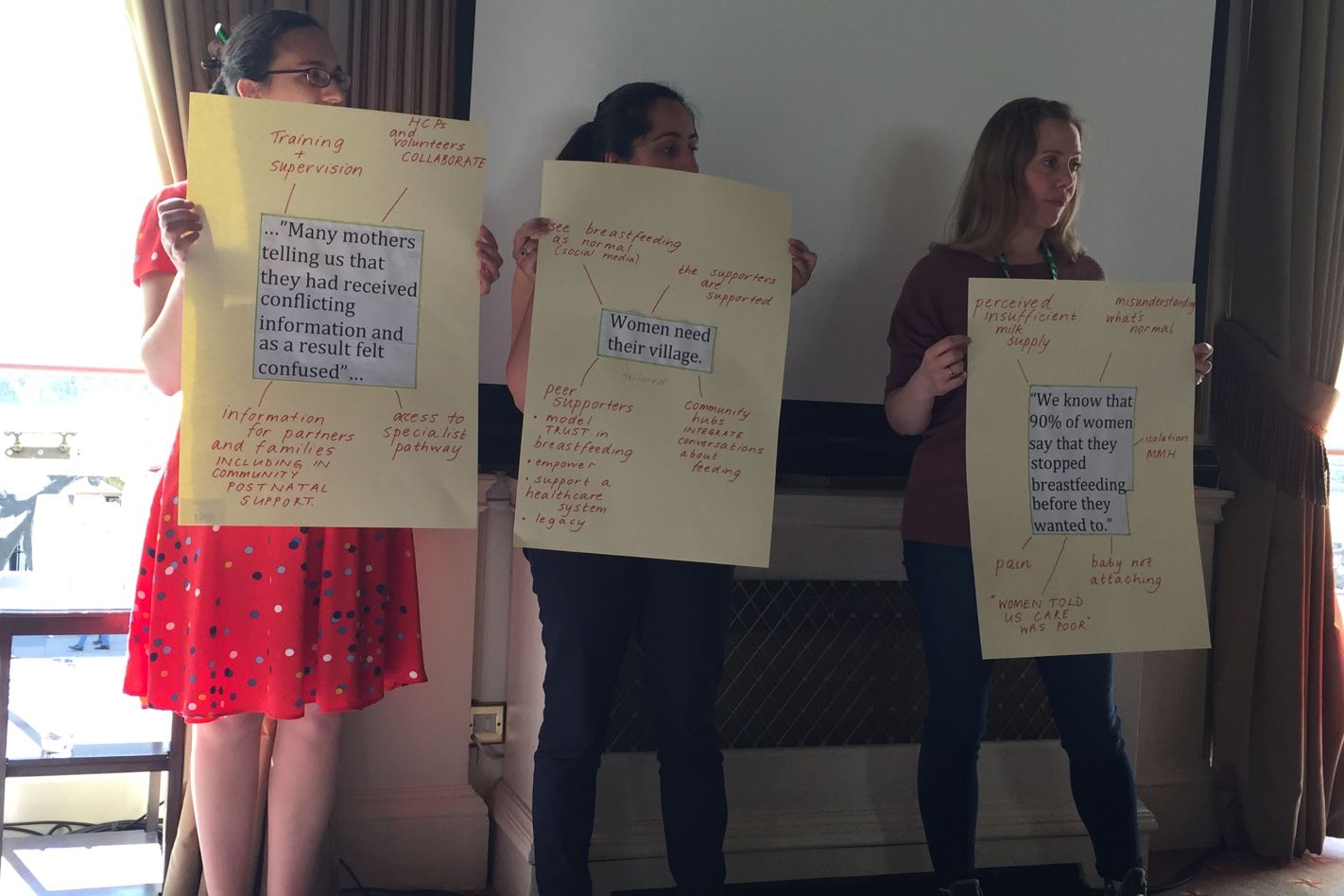
- No way of measuring UK breastfeeding prevalence
- No increased investment in child health research
The greatest areas for concern are the deepening public health cuts which have worsened in the last year and are disproportionately affecting children’s services. The scorecard marks this ‘black’, quoting latest statistics that show public health spending is over 5% lower in 2017/18 compared with 2013/14.
Professor Neena Modi, President of the RCPCH, said:
“The science exists for all to see; invest in the health of children and make a huge difference to their health in later life and hence to their economic productivity. For example, four-fifths of obese children will remain obese as adults and this will result in them losing between 10-20 years of healthy life. That’s a very frightening statistic and something that Government must get to grips with. It’s no wonder the NHS is burgeoning under the weight of ill health. This is time for a long vision for the sake of the nation’s wellbeing and prosperity yet the focus remains short-term and ineffective.”
Dr Cheryll Adams CBE Executive Director of the iHV said:
“Sadly the scorecard results are not a surprise, the Institute is repeatedly warning that cutting public health budgets is a false economy and will impact, not only on children now, but also on future generations and the fiscal spend. In particular the reduction in health visiting numbers we are seeing following such a very short lived, but exciting growth up until 2015, means that according to our own survey many children are not being seen by a health visitor at all after the 6-8 week contact. There is a research base clearly demonstrating why prevention matters and its very encouraging to see other countries responding to this by investing in child and family health. The Institute hopes that England’s ministers respond to the report by reinvesting into public health and particularly the early years and poverty reduction.”
The scorecards reveal that the Scottish and Welsh Governments are making greater strides in enacting policies to improve child health. For example, in Scotland there has been:
- The passing of the Child Poverty (Scotland) Act with defined poverty reduction targets
- A new Mental Health Strategy including a commitment to improve transition to adult services
- An announcement of plans to expand the number of health visitors by an additional 500 by the end of 2018 through the full roll-out of the Family Nurse Partnership programme
- A commitment from Scottish Government to ensure specialist breastfeeding advice and support is delivered to women
And in Wales:
- The Public Health (Wales) Act has been enacted which includes extending bans on smoking in public places to school grounds, playgrounds and NHS grounds.
- A new state of the art facility in Cardiff has opened to expand capacity for child health research
Professor Russell Viner, RCPCH Officer for Health Promotion, said:
“Child health isn’t being given the political attention it deserves in Westminster, which is disappointing given the real commitments from the Scottish and Welsh Governments. While policies such as the soft drinks industry levy and new tobacco control plan are to be applauded, the approach is piecemeal.
“Getting it right in childhood means setting up future generation for a lifetime of better health. Investing in children is an investment in the entire population.”
The RCPCH is calling for each national government to commit to a ‘child health in all policies’ approach, meaning that whenever legislation is passed, the impact on child health must be considered. The RCPCH also wants to see a cross-party committee established to develop a child health strategy.
Professor Modi added:
“We need parity of esteem between acute and preventive healthcare. It is no good only throwing money at treating established problems; there must be far better investment in prevention, which will reap immeasurable long term benefits. This means much bolder public health policies and a reversal of the current destructive cuts to preventive services.”
View the full report and summary here.