Today, the Nursing and Midwifery Council (NMC) published the latest data on the number of registered nurses and midwives, alongside intelligence on the reasons why registrants are leaving the profession. Whilst the headline message is that there are more nurses, midwives and nursing associates in the UK than ever before, the aggregate data mask a significant problem for Specialist Community Public Health Nurses, with numbers in decline.
Headline messages:
- Annual NMC data show that the number of registered nurses, midwives and nursing associates has grown by 37,723 (4.8%) to a record 826,418.
- Nearly 60,000 new nursing and midwifery professionals joined the NMC register this year alone. This was split almost equally between UK and internationally educated joiners.
- There are more nurses, midwives and nursing associates on the NMC register than ever: 826,418. That’s an increase of 37,723 (4.8 %) compared to the same period last year, and 128,184 (18.4 %) over the last five years.
- The number of leavers as a proportion of the register has fallen, but data show that one fifth of people leaving did so within ten years of joining the profession.
- After retirement, poor mental and physical health, and burnout are frequently cited reasons for leaving the professions.
SCPHN data:
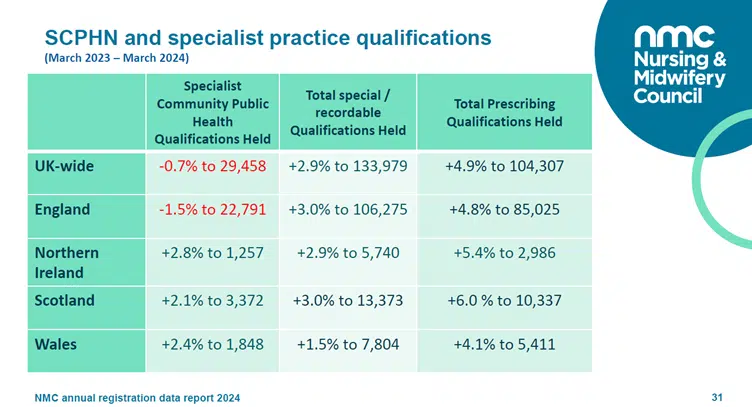
- In contrast to growth in other parts of nursing and midwifery, in England the number of Specialist Community Public Health Nurses (SCPHN) has fallen by 1.5%.
- In the devolved UK nations, there has been an increase in the number of SCPHN on the register, with a 2.8% increase in Northern Ireland, a 2.1% increase in Scotland and a 2.4% increase in Wales.
- NOTE: the number of SCPHN (health visitors) on the NMC register does not correlate with the number of health visitors working in practice. Many practitioners with a SCPHN qualification in England are now working outside the profession.
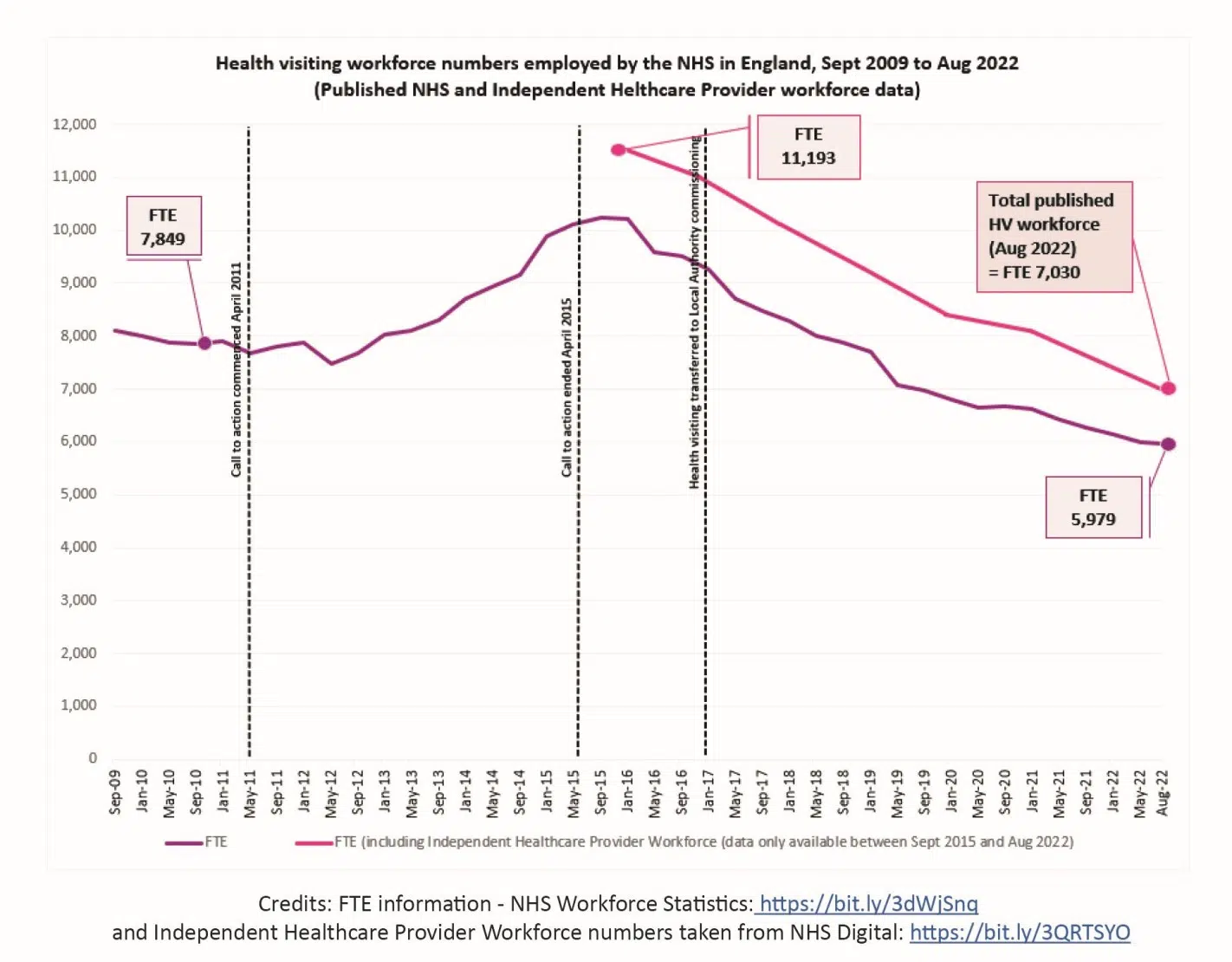
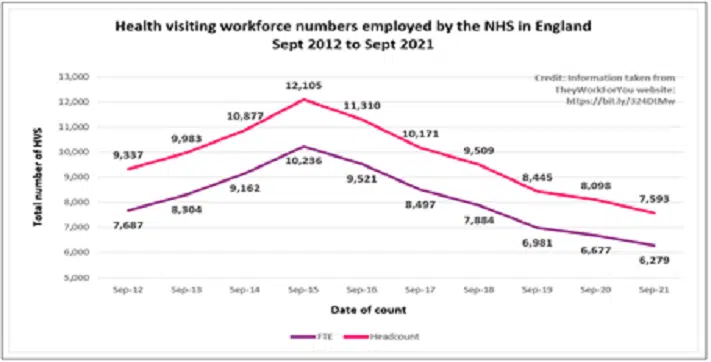
- Published workforce data on the number of SCPHN health visitors employed in England (NHS workforce data and Independent workforce data) highlight an ongoing and worrying trend, with 40% fewer health visitors employed in England since 2015 – and numbers continue to fall every year.
Commenting on the report, Alison Morton, iHV CEO says:
“The latest NMC data present a worrying picture of the ongoing depletion of the health visitor (SCPHN) workforce in England – this is easily missed in the NMC’s headline message of aggregate data showing workforce growth across nursing and midwifery as a whole.
If we are serious about prevention, early intervention and improving the health of babies, children and families – this cannot be ignored or masked any longer! England is an outlier compared to the other UK nations, with health visitor data moving in the wrong direction year-on-year. Despite health visitors’ best efforts, families with babies and young children face the brunt of these cuts, with too few health visitors to meet their needs at a time when child health is deteriorating, and health inequalities are increasing.
Today’s NMC evidence must be used by those with the power to drive change for the better. Action is urgently needed to increase the number of health visitors joining the profession and reduce the number leaving. In particular, action is needed to address the worrying trend of high workforce losses within the first few years after qualification, with better support for newly qualified health visitors to improve retention. Most importantly, we need to value these highly skilled professionals and support their wellbeing, to reduce work-related stress and poor health that is driving too many people out of the profession.”