On 30 June, the government published their long-awaited NHS Long Term Workforce Plan. The Institute of Health Visiting provided evidence and is listed as one of the organisations engaged in forming the Plan. As expected, we were keen to read the final details. The Press Release attracted considerable attention, but the ‘numbers’ in the Plan were only published later (read our initial response here).
We’ve now had a closer look – and set out ‘in brief’ the key points for health visiting and our response.
We welcome the ‘good news’:
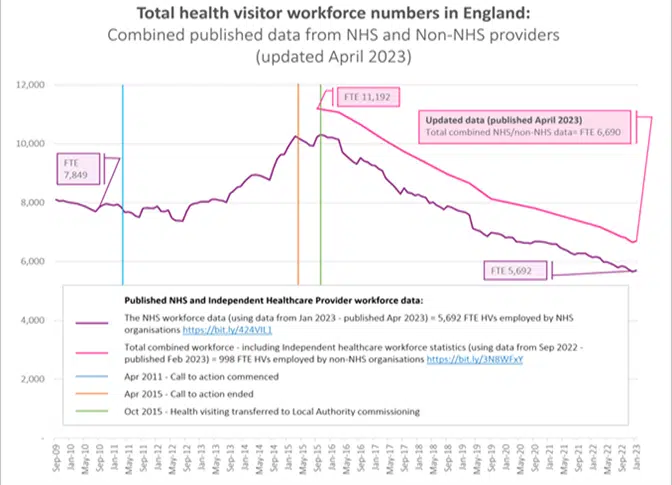
- There is a plan now! We’ve been asking for a ‘plan’ for health visiting for eight years. In that time, health visitor workforce numbers have fallen by more than 40% in England (published workforce data show a fall from 11,192 FTE in October 2015, to 6,688 FTE in April 2023).
- There is a plan that is phased with a long-term commitment! The Government has recognised that a ‘quick fix’ won’t work – we welcome the long-term and phased-nature of the Plan. It will take time to train enough new health visitors and this will need to be phased to make sure that the quality of training is not compromised. The Plan spans a 15-year assessment of the workforce that will be needed for the future (with regular reviews). It also provides a costed plan of how the current NHS workforce needs to be developed to meet the future challenges.
- The Plan extends beyond the NHS and includes health visiting! This ends some uncertainty about the future of health visiting in England that has been felt by health visitors. The profession often gets overlooked as it sits outside the NHS for its funding. The Plan, therefore, provides a welcome endorsement of the important role that health visitors play and the Government’s commitment to the profession over the longer term. It states that “The health visiting workforce is fundamental to improving the health and wellbeing of families from pregnancy to starting school by promoting health, preventing ill health and reducing inequalities. And by providing support in the community, they help alleviate pressures on hospital”.
We welcome the following commitments – but we need more details on implementation and funding:
- Retention. The Plan recognises that recruitment will not solve the workforce crisis alone. We welcome the recognition that we need to ‘embed the right culture’ to retain the highly skilled staff that we have. The Plan is light on detail for health visiting but includes important commitments to improve retention through career development initiatives, flexible working and improved staff wellbeing – this is essential, otherwise we will keep filling a leaky bucket!
- Reform. The Plan sets out the ambition to ‘work differently’ by enabling innovative ways of working, with new roles as part of multi-disciplinary teams so that staff can spend more time with patients. It changes how services are delivered, including by harnessing digital and technological innovations. As long as this improves care and outcomes, health visitors have a lot to offer in this area – the devil will be in the detail! Training will also be reformed to support education expansion, including Advanced Practice roles – we are currently working with the Department of Health and Social Care to explore how these roles could enhance health visiting. Again, more detail is needed, but in principle we are very keen to support this.
- Improving learner experience. It will be imperative that the quality of learner experience and training are not compromised. Further details are needed on how this will be managed with increased student numbers. At the last ‘Call to Action’ for health visiting, the profession was much better resourced with ‘Practice Teachers’ to oversee the placements and learning in practice. With the erosion of this role and the loss of experienced health visitors in recent years, this will need a very robust implementation plan. At the iHV, we are happy to support planning to ensure every chance of success. Clearly not having an expanded training plan is not an option. Having a phased approach will be crucial – and plans, to equip the existing workforce and Higher Education Institutions (HEIs) to manage this, need to start now!
- What about funding for substantive posts? A question we will be asking Government: ‘Will Local Authority Funding increase to support commensurate workforce expansion now and in the future?’
- What plans are there to ensure more equitable distribution of the health visitor workforce and delivery of the Healthy Child Programme across England? With many others, we continue to call for full delivery of the Healthy Child Programme, as intended, for all children, regardless of where they live.
We have some important concerns!
We’ve looked at the numbers – the Plan for health visiting is ‘too little and too slow’. The proposed trajectory for increasing student health visitor numbers will miss the mark of what is needed to rebuild an effective health visiting service:
- The Plan needs to start now, not in 2025. Without an immediate plan of action, health visitor numbers will continue to fall and families with babies and young children will face the brunt of this – too many are already missing out on the support that they need. And, for some, this has life-changing and catastrophic consequences. Health visiting service leads are already asking us how they will manage in the interim? They are ready to start now!
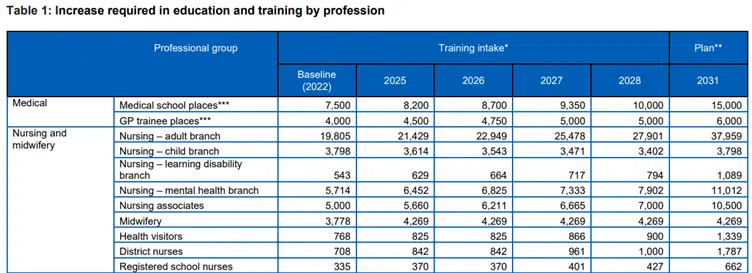
- The NHS Long Term Workforce Plan includes their assessment that education and training routes into the health visiting workforce would need to expand by between 32% and 74% by 2030/31; with an ambition to expand training places by 74% to over 1,300 by 2031/32. To support working towards this expansion, training places for health visitors will grow by 17% by 2028/29 (see Table 1 below).
- The scope is too narrow. We are not convinced that the modelling for the health visiting workforce takes full account of current demand based on population need that is recommended, or the full scope of the Health Visiting Model for England and Healthy Child Programme Schedule of Interventions. Neither does it take account of the full potential that lies within a well-resourced health visiting service to address key health, education and social care priorities across the life course (read our submission to the Major Conditions Strategy below). Health visiting is the only workforce that systematically reaches all families with babies and young children and is skilled to address a breadth of:
- physical and mental health needs for babies, children, adults and communities
- social needs
- child development concerns
- and safeguarding.
This does seem like a missed opportunity!
- The numbers are too low. Based on independent workforce modelling of health visiting by Professor Gabriella Conti in 2021, there is an estimated shortfall of around 5,000 health visitors in England.
- Health visitor workforce numbers have fallen by more than 40% since the end of the last health visitor ‘Call to Action’ in 2015 – reaching an all-time low. See graph below:
-
- Despite the boost to the workforce that is provided each year through qualifying student health visitors, on average, the health visitor workforce is still falling by 485 health visitors each year*.
- The Plan aims to train 3,416 health visitors in four years (between 2025-2028 – see Table 1).
- This is not enough – based on previous trajectories, we will need at least 750 additional health visitors a year (or 3,000 over 4 years) to just ‘stand still’.
- The net gain after 4 years at this rate will be 416 health visitors! This falls significantly short of what is needed.
- We recognise that it will take time for Higher Education Institutions to increase health visitor training places. We need a phased plan that starts this September and increases year-on-year, alongside retention, career development and return to practice initiatives to rebuild the workforce, with 5,000 more health visitors.
Summary
In summary, this Plan is a very welcome ‘step in the right direction’ that ends years of uncertainty for the health visiting profession when there was no plan. Implementing it will be a huge challenge. We recognise that there are many health visitors who were part of the last ‘Call to Action’ and gave so much of their time and energy to train large numbers of health visitors before 2015. They have been left hugely disappointed as their efforts were so easily squandered! Others are feeling exhausted working in the aftermath of the pandemic and the cost-of-living crisis. Their health and wellbeing must be a priority in these plans, and we will continue to advocate for this at the iHV.
But – this is an opportunity that the health visiting profession will need to get behind to build a sustainable future. This requires cross-party support and a long-term plan– our children’s health is too important to be left to chance and party politics!
What next: In the absence of a Chief Public Health Nurse, we have written to the Chief Nursing Officer for England, Dame Ruth May DBE, and the Public Health Minister with an offer of support and request to meet to discuss the Plan and its implications for health visiting.
Want to know more about why health visiting matters?
Read our recent evidence submissions for further details on the benefits of a sufficiently resourced health visiting workforce that will be accrued across the health, education and social care systems. Also see our infographic “Who are health visitors and what do they do?” and iHV short films – see links below:
- iHV response to Major Conditions Strategy Call for Evidence (June 2023)
- iHV submission to DfE Children’s social care strategy: Stable Homes, Built on Love (May 2023)
- iHV submission to Integration of Primary and Community Care Committee (April 2023)
- iHV submission to Health and Social Care Select Committee’s Prevention of ill health inquiry (February 2023)
- Infographic: “Who are health visitors and what do they do?” – this infographic sets out the breadth of the health visitor’s role, providing a vital infrastructure of support for babies, children and families. When sufficiently resourced, the health visiting service provides an important part of the solution for multiple cross-government department priorities for health, education and social care.
- Watch iHV Film: Health visiting in your community – a short film which showcases the breadth of health visitors’ work and their critical role in supporting the health and wellbeing of thousands and thousands of families every week.
- Watch iHV Film: Voices from practice – some health visitors share why they chose to become a health visitor and what the role means to them.
- Watch short film – Health Visitors: for every family – a short film to highlight the value and breadth of the role of the health visitor in relation to family mental health and wellbeing outcomes.
*Calculation based on published total combined HV workforce in September 2022 = 6,840; and totals combined HV workforce Sep 2020 = 7,810.

