Enabling a good learning environment for Specialist Community Public Health Nursing students in community settings is essential to equip the workforce for the future and ensure that all learners have a positive experience. The Institute of Health Visiting (iHV) and the School and Public Health Nurses Association (SAPHNA) have collaborated to produce resources for Specialist Community Public Health Nurse (SCPHN) practice learning. Our organisations invite practice learning and employer partners to pledge their support for good learning environments by adopting the Charter.
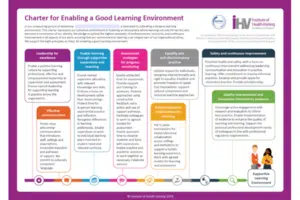
The resources have been produced thanks to funding provided by London NHS England Workforce Training and Education Directorate (NHSE WTED), previously Health Education England. The suite of resources includes a Charter for enabling a good learning environment and a self-completion maturity matrix (available in portrait and landscape formats). They are tools for communicating a commitment to quality and appraisal of education within community settings.
Learning in practice is a critical element of education and training to qualify as a specialist community public health nurse (SCPHN), a pre-requisite for registration and employment as a health visitor or school nurse within the UK. All students completing SCPHN educational programmes must, under the guidance of practice supervisors and practice assessors, demonstrate achievement of the Nursing and Midwifery Council (NMC) (2022) Standards of Proficiency for SCPHN practice1.
The NMC also stipulates requirements for the preparation and support of those supervising and assessing – indicating that each approved educational institution, and their practice learning and employer partners, must have ‘robust processes in place to support practice supervisors, practice and academic assessors prior to and throughout programmes’2. Organisations are encouraged to adopt the Charter to communicate their commitment to a culture for learning and embed eight principles into their processes for supporting practice supervisors and practice assessors.
The eight principles for a good learning environment are summarised as:
- Leadership for excellence
- Effective communication
- Enable learning through supportive supervision and teaching
- Assessment strategies for progress monitoring
- Interprofessional collaboration and learning
- Equality and anti-discriminatory practice
- Safety and continuous improvement
- Quality improvement and innovation informed by evidence
Development process
Each of the principles was identified following an appraisal of existing published research and a range of resources already used to support practice learning in the UK. The latter included NMC standards for student supervision and assessment3, the Queen’s Nursing Institute (QNI) standards for community practice teaching and education4, the NHS England safe learning environment charter5, and the Pan-London Practice Learning Environment Audit tool in use during 2023. The iHV and SAPHNA also engaged with a number of different stakeholder groups providing perspectives as students, practitioners and academics, to help shape and refine the final content of the Charter and maturity matrix. Some of those contributing were actively involved in supporting learners as either practice supervisors, practice assessors or academic assessors.
In developing the resources, stakeholders have commented:
I fully support all 8 features of the “good practice principles”. They are student-focused and learning-focused. (Health Visitor Team Lead)
I think self-assessment is a good idea and will work well. (Practice Supervisor)
It is important to include protected learning time for students and assessors, this must be valued by managers. Also, the importance of progress monitoring and ability for the student to navigate constructive feedback. (School Nurse Academic)
The maturity matrix will highlight priorities for development and will therefore be supportive for practice supervisors and practice assessors developing in their roles. (SCPHN Course Lead)
The iHV and SAPHNA invite providers of practice placements to pledge their support for good learning environments by adopting the Charter. Practitioners and teams are invited to use the maturity matrix (available in portrait and landscape formats) prior to and during provision of support for students and colleagues (new starters or those in preceptorship). The maturity matrix is a tool for reviewing professional practice and aid for planning new developments that enable learning in practice.
Jenny Gilmour, Lead supporting HEE London Improving SCPHN (HV/SN) Education Infrastructure and SCPHN Student Expansion Project, writes:
As NHSE London SCPHN (HV/SN) Education Infrastructure and SCPHN Student Expansion Project Lead, I am delighted to have commissioned and collaborated on this SCPHN Practice Learning Resource resulting in a high quality, evidence-based tool to support students in their practice placement. By highlighting essential aspects for colleagues to consider for provision of high-quality practice learning, a student experience of excellence in practice and to facilitate exposure to a positive learning environment, the tools will impact on successful student completion of the SCPHN Programme. Well supported students will, in turn, influence retention for the SCPHN Workforce going forward.
Jennifer Kirman, Principal Lecturer and Course lead SCPHN – Oxford Brookes University, and Chair of the United Kingdom Standing Conference for SCPHN Education, states:
This charter highlights the valuable aspects that make a positive learning environment. Enabling individuals and teams to self-assess against the matrix will empower a positive move to enhance the learning environment and celebrate successes to share widely with others. These resources are clear and accessible; providing an example rating will be beneficial to many in self-assessing. Thank you for this valuable charter to enhance and articulate a positive learning culture.
Helen Kimble, Senior Lecturer /Course Leader for SCPHN Programmes, University of Northampton, National Forum of School Health Educators (NFSHE) representative reviewed the resources, commenting that:
The maturity matrix will be a valuable tool alongside the Charter for guiding personal and team development and for the ongoing review of the learning environment. It provides a structured template to stimulate detailed conversations to reflect on, evidence, action plan and develop from. The maturity matrix will help teams celebrate strengths and build on any areas of weakness whilst promoting the requirements for a dynamic and evolving good professional learning environment.
Elaine Tabony, Senior Lecturer and School Nurse Field Lead, SCPHN, Brunel University London, SAPHNA Academic Advisor, notes:
The impact in signing the charter will ensure the elements of support for the student will be discussed. It clarifies expectations of both student and the assessors in practice and in university. It shows managers that there is a professional responsibility that must be adhered to.
The authors of the Charter and Maturity Matrix can be contacted at:
- Dr Karen Whittaker: [email protected]
- Julie Critcher: [email protected]
- Associate Professor Melanie Hayward: [email protected]
Please use these external links to cite these documents:
- Charter for Enabling a Good Learning Environment – https://bit.ly/4crqbc5
- Maturity Matrix for Enabling a Good Learning Environment – Landscape – https://bit.ly/4eMJ2zH
- Maturity Matrix for Enabling a Good Learning Environment – Portrait – https://bit.ly/4cLw6Za
References:
- Available at: https://www.nmc.org.uk/standards/standards-for-post-registration/standards-of-proficiency-for-specialist-community-public-health-nurses2/
- NMC 2024 Supporting information for post registration standards. Available: https://www.nmc.org.uk/standards/standards-for-post-registration/standards-for-post-registration-programmes/
- NMC 2024 SSSA Supporting information hub. Available: https://www.nmc.org.uk/supporting-information-on-standards-for-student-supervision-and-assessment/
- QNI 2023 standards for community practice teaching and education. Available: https://qni.org.uk/nursing-in-the-community/standards/community-nursing-practice-teacher-standards/
- NHS England 2024 Safe learning environment charter. Available: https://www.england.nhs.uk/long-read/safe-learning-environment-charter/