As a member of the Baby Loss Awareness Alliance, iHV supports the report published today by the Sands and Tommy’s Joint Policy Unit which makes clear that too many families continue to suffer the heartbreak of losing a baby.
The Saving Babies’ Lives Progress Report pulls together data from different sources for the first time to give everyone a shared understanding of the burden of pregnancy and baby loss across the UK. At the heart of the Saving Babies’ Lives report are the voices of bereaved parents and other family members.
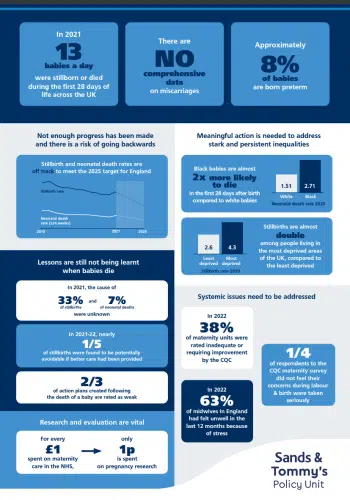
Overall, the report paints a concerning picture with progress stalling and a risk of going backwards.
In England, the Government’s target to halve the number of stillbirths and neonatal deaths by 2025 compared to 2010 levels is not on track, and there is no current target or ambition for reducing baby deaths in Scotland, Wales or Northern Ireland.
The report also highlights that despite Government commitments to act on the findings of recent reviews of maternity services, this still hasn’t led to the fundamental change needed to save more babies’ lives.
The iHV joins with others in calling for pregnancy loss and baby death to be high on the political agendas of all parties and to be treated as the urgent priorities that they are.