Research published by Swansea University this week finds that, despite their marketing claims, ‘at home formula preparation devices’ often do not deliver water hot enough (i.e. at least 70˚C) to kill bacteria that may be present in powdered infant formula.
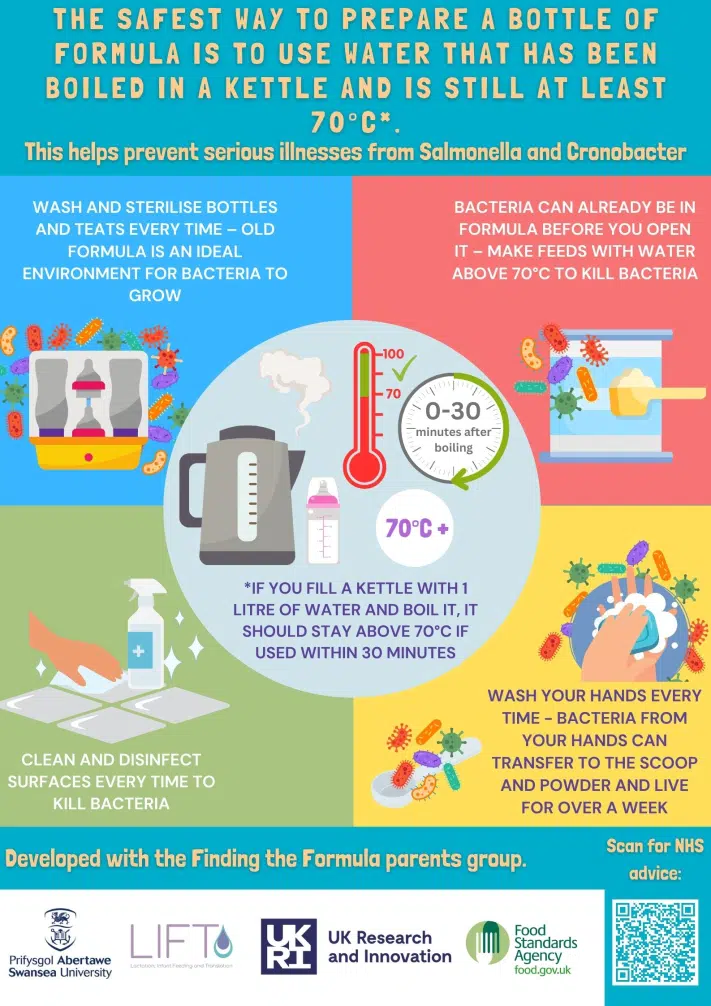
Formula-fed infants experience gastrointestinal infections at higher rates than breastfed infants, due in part to bacteria in powdered infant formula (PIF) and bacterial contamination of infant feeding equipment. The United Kingdom National Health Service (UK NHS) has adopted the World Health Organization recommendation that water used to reconstitute PIF is ≥70°C to eliminate bacteria.
The research study used community science methods to co-design an at-home experiment and online questionnaire to explore the safety of PIF preparation compared to UK NHS guidelines. 200 UK-based parents of infants aged ≤12 months were recruited; 151 provided data on PIF preparation, and 143 were included in the analysis of water temperatures used to reconstitute PIF.
Key findings:
- Only 14.9% of 74 PIF preparation machines produced a water temperature of ≥70°C compared with 78.3% (n = 54) of 69 kettle users.
- On average, preparation machine temperatures were 9 degrees C lower than when parents used a kettle.
- Most parents routinely washed and sterilised bottles and teats.
- Many parents did not always fully follow NHS safer PIF preparation guidance, including 21.8% washing their hands half the time or less, and 14.6% regularly pre-preparing bottles.
- Most parents did not appear to understand the risks of PIF bacterial contamination.
Study recommendations:
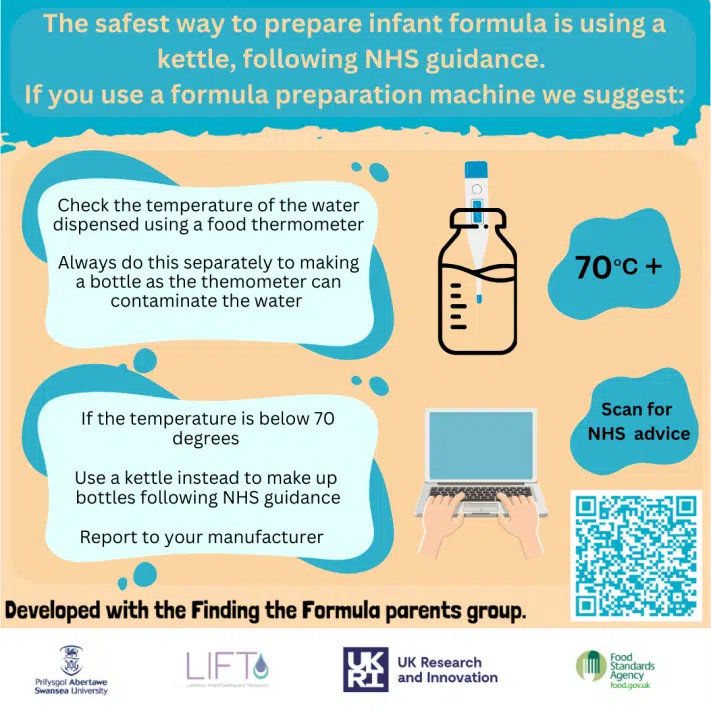
- Parents should be advised that many PIF preparation machines will not produce water that meets the minimum temperature needed to kill any bacteria present in PIF, which is not and cannot be made to be sterile.
- Instead, they should be advised to follow NHS (2019) advice, including heating water in a kettle so that it is >70°C, and, per Losio et al. (2018), ideally >85°C.
- There is an urgent need for stronger consumer protections with respect to the marketing of PIF and PIF preparation devices to further protect infants from PIF-related bacterial contamination, which can result in serious ill health and even death. This should ensure that PIF labelling is compliant with the WHO (1981) guidance (WHO Europe, 2022).
Please amplify these safety messages:
- Use the infographics produced by Swansea University and in partnership with the Food Standards Agency to share these messages widely – use them on social media, as posters, and included in teaching.
- These infographics, alongside others produced by First Steps Nutrition Trust can be found here.
Policy response:
- The Food Standards Agency (responsible for the safety of powdered infant formula) has recommended:
- All formula-feeding parents should check the temperature of the water they use.
- If formula machine users find a temperature below 70°C, they should report it to the manufacturer AND their local trading standards/Citizens Advice.
- Office for Product Safety and Standards (responsible for the regulation of formula preparation machines):
- Are conducting further testing on PIF preparation machines
- They will alert the public if any further action needs to be taken
- DHSC (responsible for content on NHS website, including bottle feeding guidance).
- No response at this stage