In the news and media this week there have been many articles about the impact of ultra-processed foods on health, including a shocking Panorama documentary on this topic. A new report published today by First Steps Nutrition Trust outlines why this significant threat to our nation’s health needs to be taken seriously for babies and young children too.
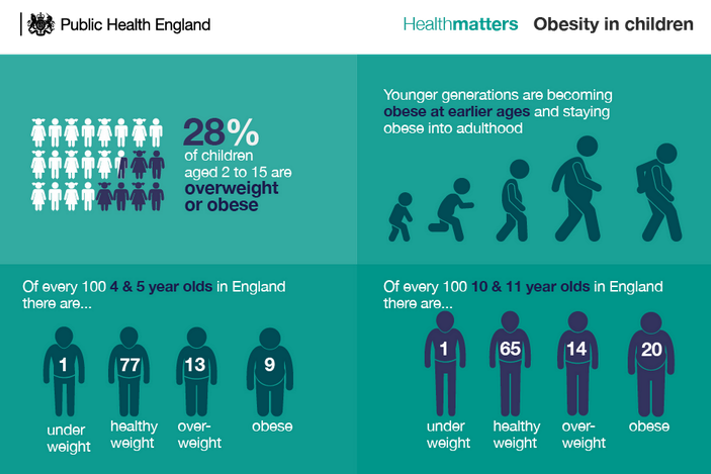
The report ‘Ultra-processed foods (UPF) in the diets of infants and young children in the UK: What they are, how they harm health, and what needs to be done to reduce intakes’ exposes how ultra-processed foods (UPF) are widely consumed, from the first weeks and months of life, raising serious concerns about the ways that they are impacting on babies’ and young children’s health and contribute to the growing obesity crisis.
The key findings from the report are stark, with evidence that all commercial formula milks and a high proportion of ‘finger foods’, snacks and baby cereals are ultra-processed. The extent of this ‘ultra-processing’ is underestimated by most people due to poor product labelling that makes it harder for parents to spot the ingredients and processing methods that are linked to health and environmental harms.
Worrying data from the report show that by 2 to 5 years of age, UPFs account for nearly two thirds (61%) of the total mean energy intake of UK children – this is higher than Australia and the USA. It is clear from the growing evidence that the impact of UPFs on our health cannot be underestimated, some of these negative health outcomes include: the promotion of overeating; disruption of developing taste preferences early in life; interference with the healthy development of the gut microbiota; and wider harmful effects due to UPFs containing certain additives and contaminants with known harmful effects.
Despite this evidence, the UK currently lacks a clear position on UPFs and companies are allowed to use aggressive and misleading marketing to promote these foods and drive high consumption levels.
Vicky Sibson, Director First Steps Nutrition Trust, called on the government to act and said:
“It is now commonplace that many babies and young children in the UK are being fed large amounts of ultra-processed foods from the start of their lives. There is robust evidence that this will be harmful to their health in the short and long term, including promoting excess weight gain.
“The Government needs to do more to enable parents and carers to feed their children diets which support healthy growth and development – based on real foods – not dominated by commercial products marketed as ‘good’ choices.
“A first step would be to explicitly address the extent to which food is processed in public health recommendations. At the same time, action to curb inappropriate and misleading marketing by the baby food industry is long overdue. The Government also needs to invest meaningfully in the health visiting service, and other facilities and benefits, to ensure that all families can get the independent, expert advice, guidance and financial support they may need to feed their children healthy diets.”
Alison Morton, CEO for the Institute of Health Visiting, said:
“Our nation is sleepwalking into a health crisis that is largely preventable, with current and future generations condemned to an increase in unhealthy life expectancy and lives cut short due to unhealthy diets and ultra-processed foods. This important report by First Steps Nutrition clearly sets out the reasons why we need to take this seriously for our babies and young children who are currently the innocent victims of the ruthless marketing of these unhealthy products that are produced specifically for them.
“Healthy foods are needed to build healthy bodies and minds. If we are to break this trajectory of declining health for our nation, we need to change the beginning of the story and ensure that all babies and young children can eat healthy and affordable food. We fully support the recommendations outlined in this report and join the call on the Government to act – our children cannot wait any longer.”
First Steps Nutrition Trust makes these seven recommendations to the UK Government:
- Acknowledge the NOVA classification and update public health recommendations on infant and young child feeding to explicitly address food processing
- Regulate and enforce the composition, labelling and marketing of commercial baby and toddler foods and drinks
- Ensure parents/carers have easy access to independent information and practical guidance and support on complementary feeding, and feeding from one to five years of age. This requires proper investment in the health visiting service and services like Family Hubs
- Ensure parents/carers on low incomes can afford to feed their infants and young children nutritious diets based on real foods by reforming the Healthy Start benefit scheme
- Enable women who want to breastfeed by increasing support, and by increasing legal protections for breastfeeding and against inappropriate marketing of commercial milk formula
- Invest in research on UPF consumption in the early years, including on additives in commercial baby and toddler foods
- Acknowledge and promote the environmental benefits of diets based on minimally processed foods
Health visitors have an important role to play in supporting parents with infant feeding and healthy diets for the whole family. iHV members can access our comprehensive ‘Healthy Weight, Healthy Nutrition Toolkit’ to support their practice here – please ensure you log into the iHV website first, to gain access.