Today, NHS England has published the first national Vaccination Strategy, bringing together all vaccination programmes, to protect communities and save lives. The strategy outlines how getting vaccinations will be made easier than ever before, including through expansion of the NHS App, ‘one stop shops’ and community outreach.
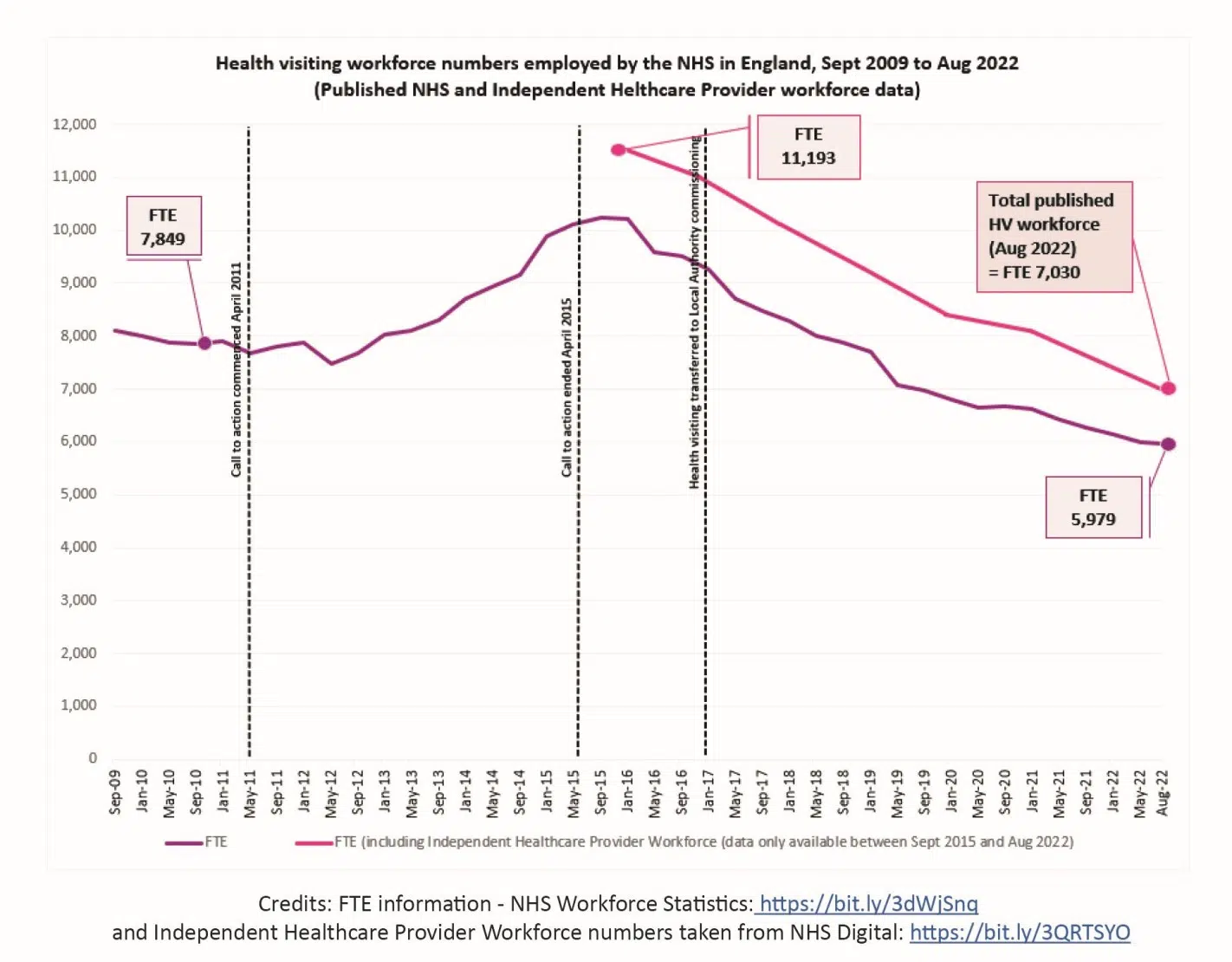
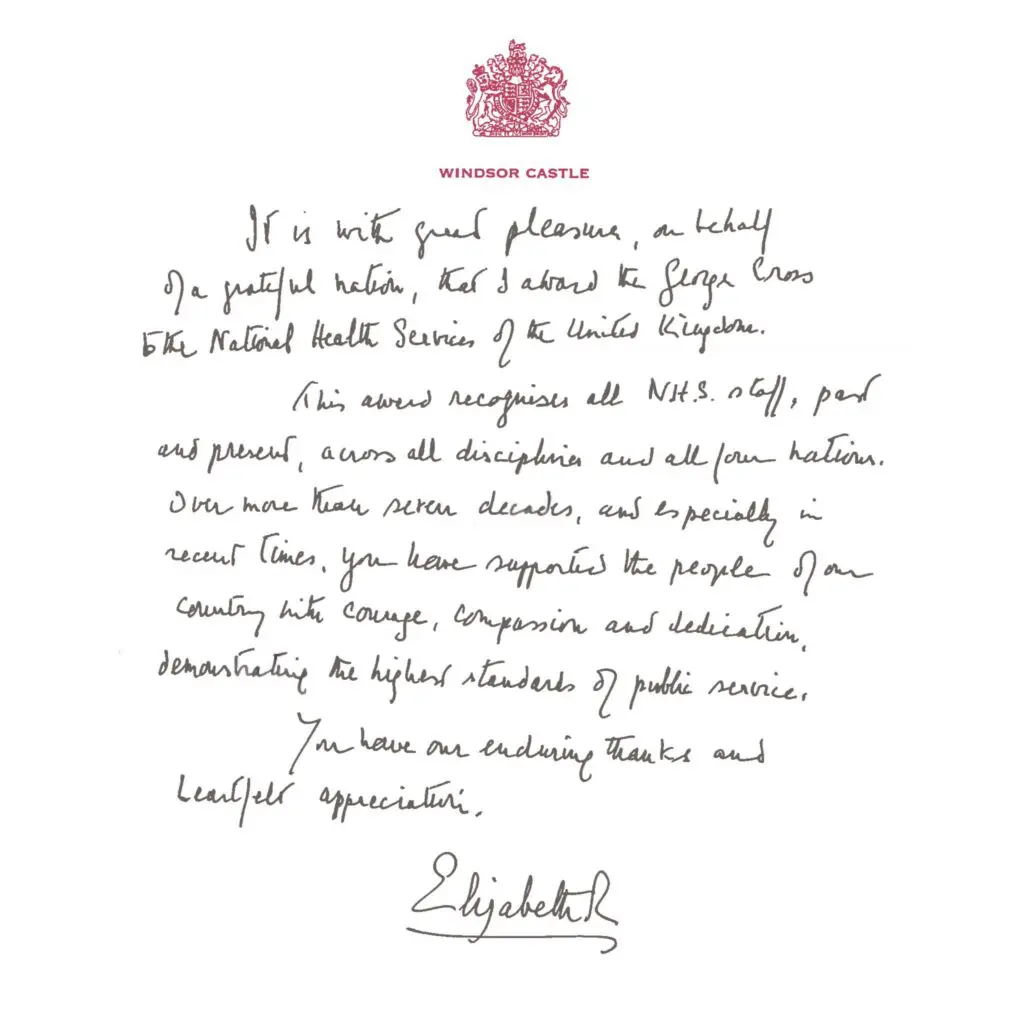
Vaccinations provide one of the most effective public health interventions, preventing between 3.5 and 5 million deaths every year across the globe through childhood vaccinations alone. Whilst the UK has a comprehensive childhood immunisation programme, falling rates of vaccine uptake over the last decade are a source of considerable concern. Tackling this issue will require a whole system approach and health visitors have an important role to play.
At the end of October, the UK Health Security Agency (UKHSA) issued an urgent letter regarding preparedness for measles resurgence in England. Measles is a highly infectious disease which can only be controlled by vaccination. Through their universal work with all families, health visitors can support uptake of the MMR immunisation programme to meet the WHO target of 95% coverage with two doses of MMR vaccine by age 5 years. Achieving this target is essential to maintain measles elimination status for the UK and prevent measles outbreaks from occurring.
The new national Vaccination Strategy outlines three clear priority areas to reverse these downward trends in vaccine uptake and prevent deaths and hospitalisations from vaccine-preventable diseases. These include:
- Improving access including an expansion of online services: Many more people will be able to book their vaccines online quickly and easily, including via the NHS App. Families will be able to view their full vaccination record with clear information and guidance on what vaccinations they should have to keep them well.
- Vaccination delivery in convenient local places, with targeted outreach to support uptake in underserved populations: Bespoke outreach services should be tailored to communities that are un- or under-vaccinated, building trust and confidence.
- A more joined-up prevention and vaccination offer: Vaccination services and activities should be holistic, offering multiple vaccinations for the whole family where appropriate.
The Strategy sets out its plans for improved integration with clinical pathways and greater joint working across all local service providers, including acute, community, mental health and local authorities. Systems should consider how they can:
- Make vaccination the business of everyone working in patient-facing settings, through training and awareness campaigns. This includes using key contacts to talk to the person about relevant vaccinations, answer questions and, if they cannot deliver the vaccination there and then, signpost to the appropriate services.
- Base vaccinators in healthcare settings accessed by people who may benefit most from vaccination. This may include emergency departments, outpatient departments, family hubs and community diagnostic centres. The report highlights that, “Family hubs may be especially beneficial for babies and children where parents may be less likely to access a standard offer.”
- Train and deploy a wider set of professionals to deliver vaccinations. The reports states that, “Local authority services for 0–5 year-olds, for example, have unparalleled contact with underserved communities. Health visiting teams as well as school nursing teams have successfully delivered vaccinations in the past and continue to do so in parts of the country, making use of their extensive skills and relationships. Any such arrangements would need to be locally planned and take into account workforce capacity and funding requirements.”
Whilst the Vaccination Strategy does not set out all the specifics of implementation (and there will be a range of considerations that will need to be addressed), NHS England has indicated that they will continue their work with stakeholders (including the iHV) to develop their plans in order to deliver the proposals. With sufficient resource, there are significant opportunities to build on the work that has already started in Integrated Care Systems to provide more ‘joined-up’ vaccination programmes in the future, across the whole pathway including through integrated neighbourhood, place and system teams. We are particularly pleased to see the emphasis on reaching all parts of the community, with a specific focus on underserved and marginalised communities that will be needed to tackle widening health inequalities.
Professor Helen Bedford, Professor of Children’s Health, Population, Policy and Practice Programme, UCL Great Ormond Street Institute of Child Health and iHV Expert Adviser: Immunisations, commented:
The UK vaccination programme is among the most successful worldwide, yet there is room for improvement to ensure we offer maximum protection to the population against infectious disease. Each year for the past ten years, small declines in uptake of childhood vaccines, together with large disparities in uptake between geographical areas and social and economic groups, are a cause for concern. If fully implemented, the Vaccination Strategy will be vitally important to ensuring we improve our current position and placing us well to maintain the success of the programme into the future. Through their contacts with families, and the trusting relationships they build, health visitors play a key role in boosting vaccine confidence and in securing the success of the childhood vaccination programme.
Read iHV Good Practice Points: Promoting the Uptake of Childhood Immunisations which contains advice on health visitors’ role supporting vaccination uptake as part of an integrated approach.