Just before the end of 2022, the iHV celebrated its 10th birthday and, reflecting on those years, we feel incredibly privileged to have worked alongside so many inspiring people. Year on year, the iHV Mental Health Team has been part of some phenomenal partnerships, delivering a difference for families – and this last year is no exception. Thank you to you all.
Our Mental Health Team report, published today, looks back and celebrates what we have collectively achieved from January 2022 to January 2023 – despite the challenges. We hope you enjoy it – and we hope that during 2023, as part of enabling your own wellbeing and future successes, you also take the time to celebrate your achievements.
Reflecting on the last 10 years, Melita Graham, iHV Head of Mental Health Dept, said:
I came into the iHV because I believed it was the organisation that would offer me the most opportunity to make the biggest difference, in my lifetime, to the lives of babies and their families. After 10 years, my conviction is even stronger, and without exception, each member of the iHV Mental Health Team shares this belief.
Such a lot has happened in the world in the last year and with the pivot to online working, beside the increased need of mental health support for families because of the pandemic, the cost-of-living crisis and widening inequalities, the professional pace of life is staggering.
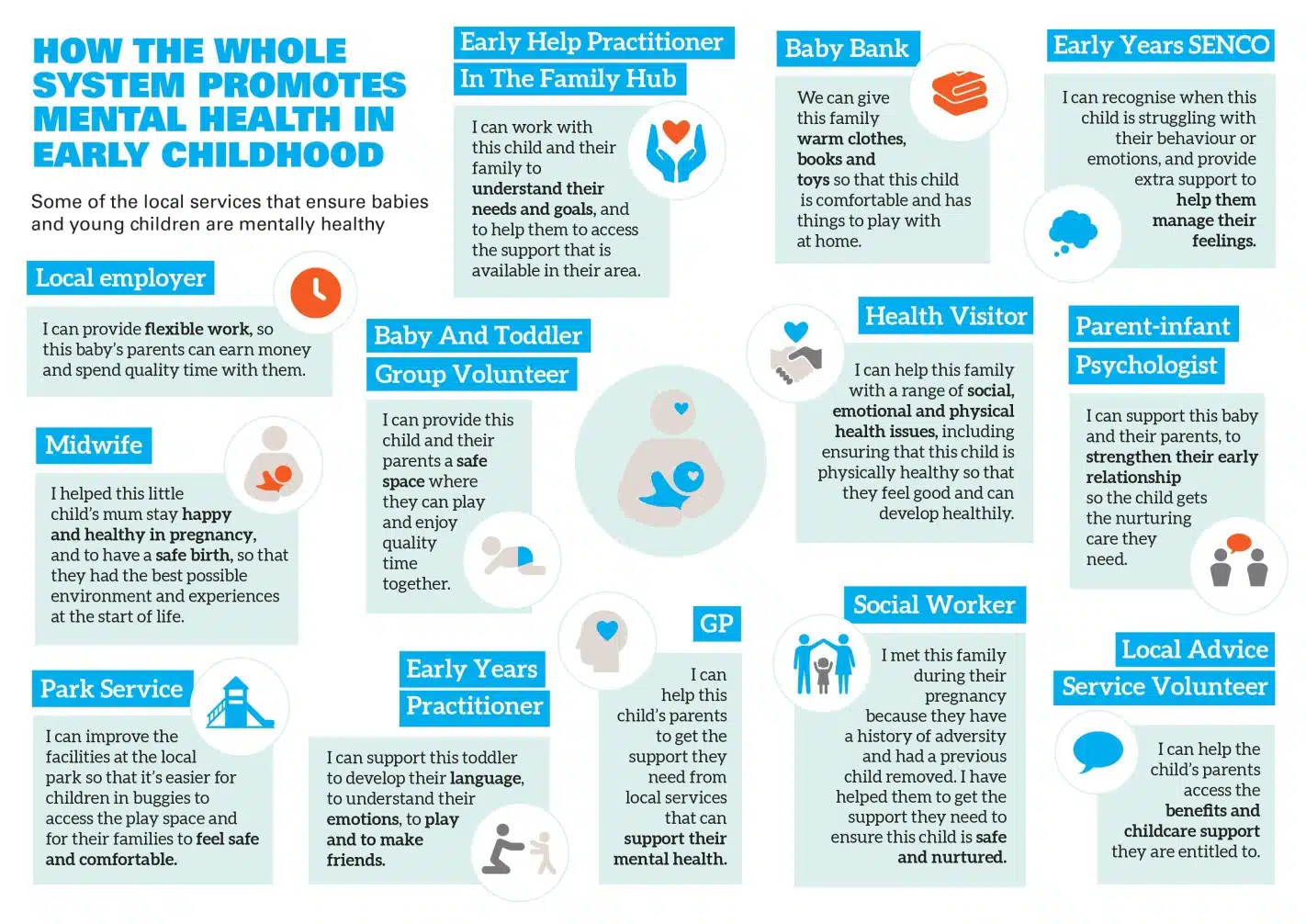
Throughout 2022, we have stayed close to health visitors and iHV Champions on the ground, parents with lived experience and our partner organisations. We know how tough it is for families and for health visitors and our partners across the mental health system supporting families. The iHV Survey 2022 makes for sobering reading and the 2022 MBRRACE report yet again showed that suicide is still the leading cause of death for women when looking across the perinatal period. Both reports add weight to the mounting evidence of the unacceptable and preventable widening inequalities across the UK.
The iHV has worked hard alongside you in 2022 to drive change and, going into 2023, we are deeply committed to making sure that the voices of babies and their families are heard. Alongside our partners, we won’t stop until every family, irrespective of where they live, has access to a health visitor who has the right qualities, competence, and capacity to deliver high-quality, personalised, and compassionate family mental health care.
To achieve this, we must make self-care for ourselves and each other a priority. All too often, we move on to the next thing without stopping to acknowledge and consider the challenges overcome, the distance travelled, the differences we have made, and what we need to sustain our energy and our hope for the future. At our final iHV Perinatal and Infant Mental Health Forum in December 2022, iHV PIMH Champions came together and celebrated what they had achieved – despite the challenges. Each one of us went away feeling more supported, buoyed, re-energised and inspired! We are all looking forward to building our connections in 2023 and beyond.
Alison Morton, Executive Director iHV, said:
“I am delighted to see today’s report published which sets out the phenomenal achievements of the iHV’s Mental Health team in the last 12 months. Supporting families’ mental health is a priority for the Institute and for the nation – we are privileged to have such a highly skilled team leading this work. Congratulations to each member of the iHV’s mental health team for their achievements and Melita Graham for her inspiring leadership.
“I hope that you will enjoy reading today’s report which showcases the numerous award-winning and innovative PIMH programmes that are being delivered across the UK by the iHV, and in partnership with others, to support practitioners in their work with families and better mental health across the lifecourse.”