The Institute of Health Visiting (iHV) publishes a pathway for a career in health visiting.
Across all UK nations, governments are looking to build a health and care workforce fit for the future. This includes responding to changes in our population’s needs and investing in prevention and public health to ensure that people can live longer, healthier and happier lives. There is also much greater awareness of the evidence for investing in the earliest years of life as a critical period to build strong foundations for future health and reduce the risks for diseases that are largely preventable – it is clear that health visitors are needed now more than ever.
But, at the same time, we have significant workforce shortages in health visiting, which is impacting on parents’ experience, service capacity and constrains our ability to transform services to improve support for families with babies and young children. Rebuilding the workforce will take time. The solution rests on building worthwhile and attractive career opportunities in health visiting at all levels – whether practitioners are just entering the field or looking to progress in the profession to more senior roles.
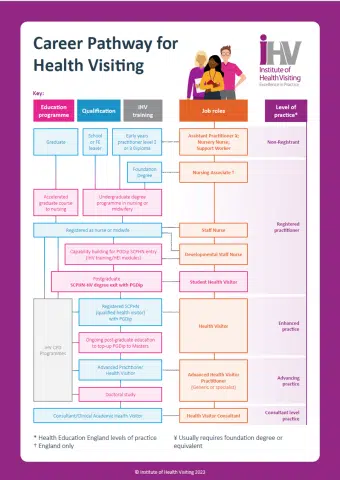
Our career pathway sets out health visiting career options. It draws on the NHS Long Term Workforce Plan’s priorities to “train, retain and reform” in order to build workforce capacity and capability and support practitioners to have worthwhile careers in health visiting.
Health visiting is a form of public health practice dedicated to creating good health. Health visitors embrace strengths-focused relational approaches and take account of the setting and circumstances impacting on a person’s life. These features, and the primary goal of health creation, define health visiting as a distinctive form of nursing and is an area of public health within which a whole career can be grown.
The Career Pathway for Health Visiting has been designed as a resource for workforce planning. It includes the different job roles contributing to health visiting provision and maps these against levels of practice that reflect registration status, educational development, expertise, and responsibility.
The downward trend in total health visitor workforce numbers in England needs urgently addressing (see our news story Health visiting in the NHS Long Term Workforce Plan: In brief). The NHS Long Term Workforce Plan published in June 2023 signals a commitment to address the shortfall, which needs action not only on recruitment but also retention. The iHV recognises the use of skill mix roles and has developed the career pathway with entry and progression in mind. It sets out possibilities for movement towards a health visitor qualification and beyond, through advanced practice.
The imperative is for employers to invest in new talent and harness expertise whilst helping individuals see where their ambition can take them when health visiting is their chosen career.
More details about the Career Pathway in Health Visiting will be shared by Dr Karen Whittaker at the iHV Leadership conference on 6 December 2023 – an event that can be joined in-person or online (in-person ticket sales close Friday 24 November). See https://ihv.org.uk/events/leadership-conference-2023/ for booking details.
To cite this infographic, please use the link to the pdf here: https://bit.ly/47GEm9Q
Please also see:
- ‘Becoming a health visitor’ to consider how to prepare for education and training as a health visitor;
- Our short iHV films “Health visiting in your community” and “Voices from Practice” to gain an insight into the breadth and depth of health visitors’ work with every family.