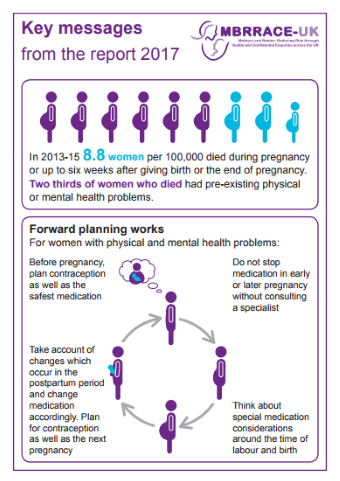
Today, MBRRACE-UK published their latest Confidential Enquiry: MBRRACE-UK Saving Lives Improving Mothers’ Care – Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2018-20. For many years suicide has been the leading cause of direct deaths in the year after pregnancy. We are deeply concerned that this has not changed, indeed, the latest report shows that mental ill-health is an increasing cause of maternal death.
Key perinatal mental health findings:
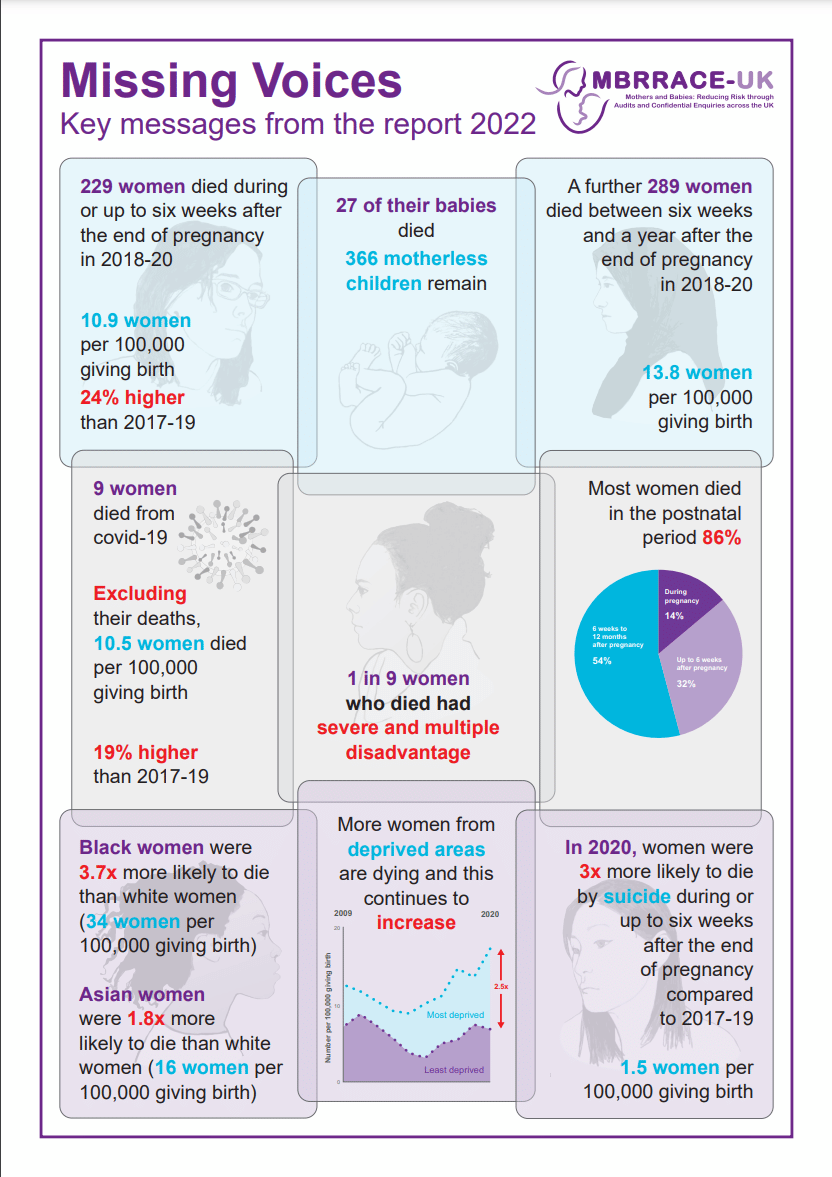
- 1 in 9 mothers who died experienced severe and multiple disadvantages, such as mental illness, domestic abuse and substance use
- More women from deprived areas are dying and this continues to increase
- 40% of deaths within the year after pregnancy were from mental health-related causes
- Suicide remains the leading cause of direct maternal death in the first postnatal year
- Suicide during pregnancy or up to six weeks after is increasing – in 2020, women were three times more likely to die by suicide during this period compared to 2017-19
- Very few women who died by suicide in 2020 had formal mental health diagnoses, but significant numbers had a history of trauma
- Women living in the most deprived areas are more than twice as likely to die as women living in the wealthiest areas
- Concerning trend of increasing teenage suicides
- Roughly doubling of domestic abuse rates in suicide and substance misuse deaths, compared to 2017-2019.
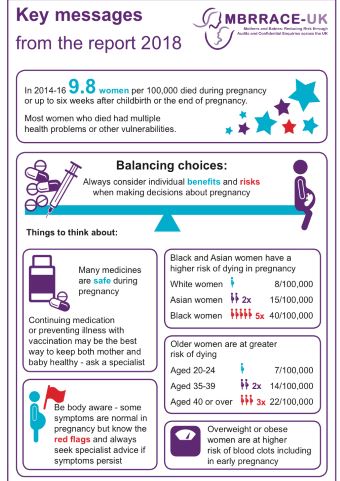
There remain gaps in mortality rates between women from deprived and affluent areas, women of different ages and women from different ethnic groups. Although there has been some positive improvement, this year’s report still shows a continued gap between the mortality rates for women from Black, Asian, mixed and white ethnic groups, with:
- a more than three-fold difference in maternal mortality rates among women from Black ethnic backgrounds, compared to white women
- an almost two-fold difference amongst women from Asian ethnic backgrounds, compared to white women.
Responding to the report and its recommendations, Melita Walker, Head of Mental Health at the Institute of Health Visiting, said:
“We are again deeply saddened by the latest MBRRACE report and offer our heartfelt sympathy and deepest condolences to all the families who represent the ‘human face’ of these stark statistics.
“It is worrying to hear, yet again, that suicide is still the leading cause of direct maternal deaths in the year after pregnancy and of the continuing impact of health inequalities on the lives of so many. If we are to save lives, we must work together to make sure that all families have access to the same high-quality mental and physical healthcare. This requires putting families at the centre of a whole system approach with fully integrated systems of care working well together.”
We would like to acknowledge the importance of these powerful reports in facilitating change and enabling systems to work together to address inequalities and the unacceptable tragic outcomes for families. The sound evidence from MBRRACE, alongside the tragic real experiences of the families that the MBRRACE reports bring sharply into focus, provides the foundation for the iHV Champions mental health training modules on risk and inequalities. We act with urgency to get the lessons from MBRRACE into practice and have now trained 3,900 Multi-Agency Champions. We are confident that sharing this learning is making a difference and saving lives – but we know we need to do more.
“Having attended the launch today I have come away more determined to shine a light on the importance of maximising the health visitor role in this area. As a system we must urgently reflect on the learning, including that: in 2020, women were 3 times more likely to die by suicide during or up to six weeks after the end of pregnancy compared to 2017-19; the majority of deaths by suicide and mental health causes occur later in the first postnatal year; and very few women who died by suicide in 2020 had formal mental health diagnoses, but significant numbers had a history of trauma.”
Health visitors are there for every family throughout the perinatal period and beyond. As such, as part of the “whole system”, health visitors play a vital role in building trusting relationships with families, identifying and responding to mothers at risk, offering pro-active, evidence-based and life-saving interventions, including timely referral on to specialist services when needed. But they can only do this effectively if they (and the whole perinatal mental health system workforce) are available in sufficient numbers, with the right training and capacity. We know we need more health visitors and, more importantly, we know that mothers and their families need them.
The iHV remains deeply committed to addressing inequalities and driving change. Alongside our partners, we won’t stop until every family, irrespective of where they live, has access to a health visitor who has the right qualities, competence, and capacity to deliver high-quality, personalised, and compassionate mental health care.