iHV joins a group of 8 leading health organisations in publishing and sharing a consensus statement calling for the Government to urgently act to reverse increasing inequality in children’s oral health.
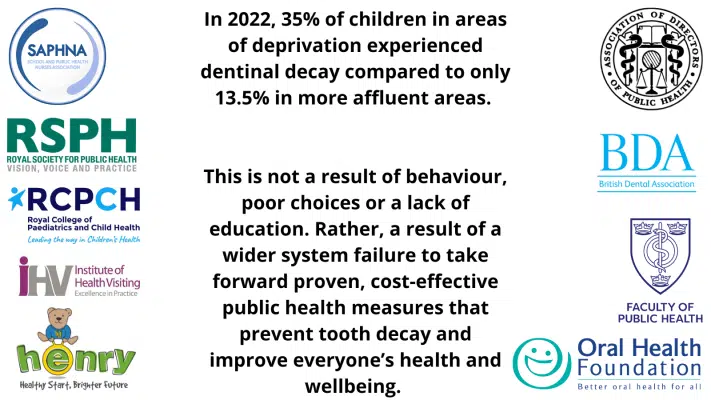
A survey of oral health in five-year-old children, produced as part of the National Dental Epidemiology Programme and published last week, found that over 35% of children in areas of deprivation experienced dentinal decay in 2022 in comparison to only 13.5% in more affluent areas.
With tooth decay the leading cause of hospital admissions for five-to-nine-year-olds, there is a significant, and preventable, knock-on cost to the NHS.
Families do need to be equipped with the knowledge to encourage and oversee good hygiene practice amongst children. However, this report’s worrying findings are not a result of behaviour, poor choices or a lack of education. Rather, they are a result of a wider system failure to take forward proven, cost-effective public health measures that prevent tooth decay and improve everyone’s health and wellbeing.
We therefore urge the Government to:
- Impose further restrictions on the marketing and sale of sugary food and drinks.
- Support policy across all departments to improve access to affordable, healthy food.
- Increase the number of water fluoridation schemes, which are the single most effective public health measure for reducing tooth decay rates.
- Improve access to fluoride varnish programmes.
- Facilitate timely access to free child dental services for preventative advice and early diagnosis.
- Ensure that the early years workforce are educated about the importance of child oral
Signatories:
- Professor Jim McManus, President, Association of Directors of Public Health
- Eddie Crouch, Chair, British Dental Association
- Professor Kevin Fenton, President, Faculty of Public Health
- Kim Roberts, Chief Executive, HENRY
- Alison Morton, Chief Executive Officer, Institute of Health Visiting
- Dr Nigel L Carter, Chief Executive, Oral Health Foundation
- Dr Helen Stewart, Officer for Health Improvement, Royal College of Paediatrics and Child Health
- William Roberts, Chief Executive Officer, Royal Society for Public Health
- Sharon White OBE, Chief Executive Officer, School and Public Health Nurses Association



