Invest in Childhood: new report calling for Government action to prevent mental health problems in babies, children and young people.
The Centre for Mental Health has launched a new report focused on the critical issue of mental health for babies, children and young people and the imperative of addressing mental ill-health. The Invest in Childhood report sets out how the Government can act now to prevent mental health problems among children and young people. It explores the available evidence about how government can use its powers to boost family mental health, investing in what works and how to most effectively direct resources.
Invest in Childhood says that the Government can turn around the rise in mental health problems among children through evidence-based, cost-effective prevention strategies. The report identifies six critical areas for immediate action, from the perinatal period and early years, to schools and colleges, and through to entering the job market.
Of particular note to health visitors is the recommendation for expansion of the workforce and recognition of the unique role health visitors play in promoting good emotional health and wellbeing of the whole family. The report says that health visitors play a vital role in promoting good mental health in children and families, and in spotting the signs of mental health difficulties early. However, it recognises that the profession has faced successive cuts to the workforce, meaning that more children fall through the gaps of early support and go on to need specialist care. Invest in childhood calls on the Government to take action now, saying that boosting the number of health visitors will benefit babies, children and families for decades to come.
‘Health visiting is a cornerstone of early childhood support, offering a unique opportunity to engage with families during the formative years of a child’s life’
(Invest in Childhood report, 2025)
The report recommends the following:
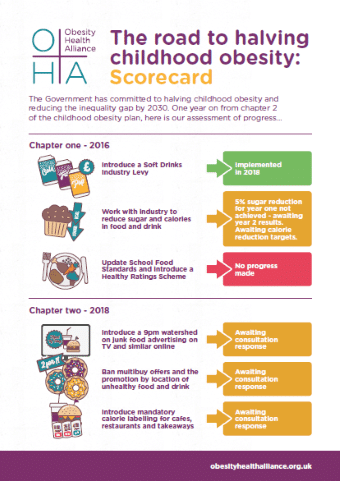
- The UK Government should take steps to tackle the social determinants of children and young people’s mental health. Current legislation to improve workers’ and renters’ rights are welcome measures towards this aim. Action to tackle violence against women and girls, child poverty, and racial injustice will further address some of the biggest drivers of mental ill health among children and young people today. A whole government mental health strategy, backed up with a mental health policy test and a Mental Health Commissioner, would strengthen the machinery of government so that future policies are made with children’s mental health in mind.
- The UK Government should create a nationwide programme to invest in community-led mental health promotion and mental illness prevention activity. This could be modelled on the Better Mental Health Fund, to enable local councils across the country to support community initiatives to improve children’s mental wellbeing. This should focus on the most disadvantaged and marginalised neighbourhoods and groups of people in each locality.
- The UK Government should invest in evidence-based parenting programmes, adopting a proportionate universal approach with a low-cost offer for all and additional help for those who need it. Some local and combined authorities have begun to implement this locally.
- The UK Government should improve mental health support for mothers during the perinatal period, building on the expansion of specialist community services to provide a more comprehensive support offer.
- The UK Government should expand the health visitor and school nursing workforce. Public health nurses play a vital part in supporting children’s mental and physical health, and as such are a good long-term investment.
- The UK Government should support early years education settings, schools, colleges and universities to adopt a whole education approach to mental health. Applying a mental health policy test to education policies would further embed the whole school approach by providing greater consistency and evidence-based policies, for example around the curriculum and the ways behaviour and attendance are managed in schools.
- The UK Government should fulfil its manifesto pledge to establish an open access mental health hub in every community in England. These will provide early support for young people’s mental health, and also help with housing, employment and other essentials for young adults up to the age of 25 making the transition to working life. These issues should be central concerns of the Government’s forthcoming Youth Strategy
Hilda Beauchamp, PIMH Lead at iHV, said:
“This timely report draws our attention, again, to our most vulnerable citizens. The declining mental health of babies, children and young people in England requires an urgent, informed and co-ordinated response, especially in the current context of economic and global instability. We welcome the Centre for Mental Health’s recognition of the pivotal role that health visitors play in identifying early signs of mental health difficulties in babies and young children and providing essential support and early intervention to families. We would urge the Government to heed the evidence highlighting the clinical and cost-effectiveness of a well-resourced health visiting service and respond urgently to the recommendation to expand the workforce.”
The report concludes that the evidence is clear: to secure a brighter future for babies, children and young people, we must invest in childhood. By harnessing the possibilities that technology brings, building on the evidence of what makes a difference, and creating health-enhancing environments, we can empower young people and families, support educators, and tackle the broader challenges of disadvantage. These actions are essential steps towards preventing mental health problems and fostering a generation of young people who are healthy, resilient, and capable of achieving their full potential.
Read Institute of Health Promotion and Education Rapid Response to report published in BMJ: