21st June 2019
Our final blog for National Breastfeeding Celebration Week 2019 #CelebrateBreastfeeding is from Dr Wendy Jones MBE Breastfeeding and Medication Pharmacist. Wendy also presented at our recent evidence-based practice conference in Manchester.

Dr Wendy Jones MBE Pharmacist
When I first wrote information on the safety of drugs in breastmilk back in 1995, I didn’t know how it was going to change my life. Since that time, I have met literally thousands of people keen to hear how we balance the risks and benefits for mums who are unwell but are also breastfeeding so that the baby may also be exposed. Having had a new grandchild born just last week has given me another perspective of how my daughter (who has been brought up with me wittering on about the subject) has approached pain medication following her c-section.
I rely on people such as those I met at the iHV conference, to spread the word that breastfeeding mothers can have medication to treat almost every condition and continue to breastfeed as normal. The information in the BNF can only be taken as a guide and needs additional data from specialist sources to evaluate the risks. Telling a mother to stop feeding her baby is also fraught with risks from potential mastitis in mum or dehydration in the baby who may refuse to feed from a bottle or accept formula milk.
I provide information to around 10,000 mothers and professionals a year varying from the use of nail varnish to snorting cocaine. Health visitors are trusted and accessible sources of information. Sometimes from queries I receive, they are the go-between when mothers find doctors are intimidating or possibly less than supportive of breastfeeding because they haven’t had the training on feeding that health professionals have.
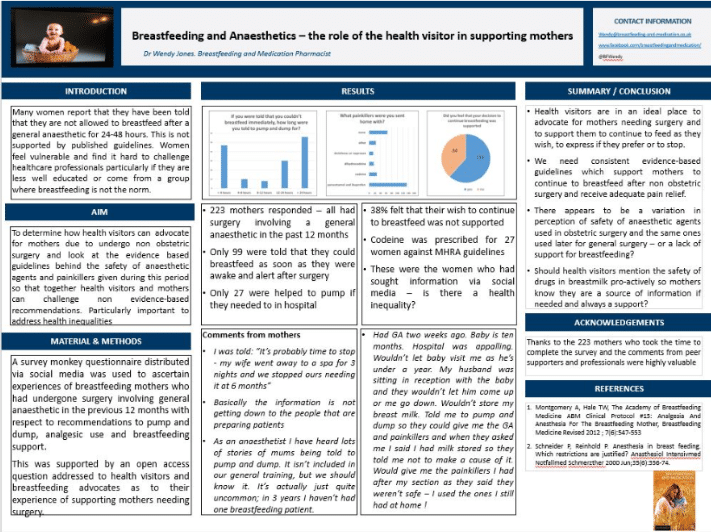
It was my pleasure to present to the iHV conference about the results of a small survey I conducted via social media on general anaesthetics and breastfeeding. It seems that advice on painkillers, feeding after a general anaesthetic and support on the wards is very different between a maternity ward and a general surgical ward. Mothers reported that 55% were told that they could feed as soon as they were awake and alert after surgery, compared to the standard care after a c-section under a general anaesthetic. Only 13% were helped to pump their milk and commented that wards were unsupportive of babies being on the ward to breastfeed even with the support of another adult. 70% were sent home with painkillers with the majority getting simply paracetamol and ibuprofen although over 10% were given codeine – a drug no longer recommended for breastfeeding mothers.
The aim of my presentation at the iHV conference was to look at how health visitors might prepare their clients who need surgery and provide them pro-actively with signposts to further information
https://breastfeedingnetwork.org.uk/wp-content/dibm/anaesthetic%20and%20breastfeeding.pdf
https://www.breastfeeding-and-medication.co.uk/thoughts/breastfeeding-and-anaesthetic
I get many emails from health visitors every week and I am always happy to provide information on the medication or procedure their clients need. I feel that their input is much under valued and I wish we could emphasise the value of their input to breastfeeding.
So, as we celebrate Breastfeeding Week, I want to raise a toast to all the unsung individuals who day after day support new mums in what can be a challenging time in their lives. Thank you for giving me the opportunity to contribute this blog.
Dr Wendy Jones MBE Breastfeeding and Medication Pharmacist